Respiratory Failure
Respiratory failure occurs when the respiratory system fails in either one or both of its gas exchange functions: oxygenation and the elimination of carbon dioxide. A reduction in the oxygen carried in the bloodstream is referred to as hypoxaemia, and a rise in the carbon dioxide levels within the bloodstream is referred to as hypercapnia.
Respiratory failure is classified into two groups
- Type I respiratory failure
- Type II respiratory failure
Type I respiratory failure
Type I respiratory failure occurs when there is a problem with oxygenation resulting in hypoxaemia. This is most commonly caused by ventilation/perfusion mismatch resulting in reduced diffusion of oxygen from the alveoli into the pulmonary circulation. Type I respiratory failure is characterized by
Type II respiratory failure
Type II respiratory failure occurs when there occurs when there is inadequate alveolar ventilation resulting in hypoxaemia and hypercapnia. Type II respiratory failure is characterized by
Type II respiratory failure can be further sub-classified depending on the pre-existing condition of the patient and the speed of onset
Acute type II respiratory failure
The patient will have no, or minor, evidence of pre-existing respiratory disease and patients typically have a high PaCO2, low pH, and normal bicarbonate.
Chronic type II respiratory failure
Evidence of chronic respiratory disease, high PaCO2, normal pH, and high bicarbonate (>26 mmol/l).
Acute-on-chronic type II respiratory failure
An acute deterioration in an individual with significant pre-existing type II respiratory failure, high PaCO2, low pH, and high bicarbonate (>26 mmol/l).






















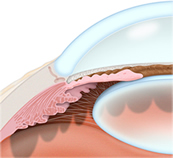 Open-angle glaucoma is the most common type of glaucoma where the fluid in the eye drains too slowly through the network of tiny drainage channels, known as the trabecula. The pressure in the eye increases as the fluid in the eye continues to build. Loss of vision occurs gradually and the vision loss is not always noticed until it becomes irreversible. About 95 percent of glaucoma cases are due to open-angle glaucoma.
Open-angle glaucoma is the most common type of glaucoma where the fluid in the eye drains too slowly through the network of tiny drainage channels, known as the trabecula. The pressure in the eye increases as the fluid in the eye continues to build. Loss of vision occurs gradually and the vision loss is not always noticed until it becomes irreversible. About 95 percent of glaucoma cases are due to open-angle glaucoma.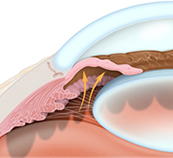 Angle-closure glaucoma occurs when the tiny drainage channels, known as the trabecula, become blocked which then causes a sudden rise in pressure in the eye. This condition is not common but when it occurs it requires immediate medical attention.
Angle-closure glaucoma occurs when the tiny drainage channels, known as the trabecula, become blocked which then causes a sudden rise in pressure in the eye. This condition is not common but when it occurs it requires immediate medical attention.



